Hamza Asumah, MD, MBA
In the realm of healthcare, interoperability is not just a buzzword; it’s the cornerstone of efficient operations and high-quality patient care. As medical technology advances, healthcare providers, payers, and patients are all increasingly reliant on a complex web of electronic health records (EHRs), digital prescription services, telemedicine platforms, and other health IT systems. Despite the potential of these tools to revolutionize patient care, the road to seamless interoperability among healthcare systems remains fraught with challenges. In this blog, we delve into the issues surrounding healthcare IT interoperability and explore the implications for operational efficiency and patient outcomes, supported by relevant data and research.
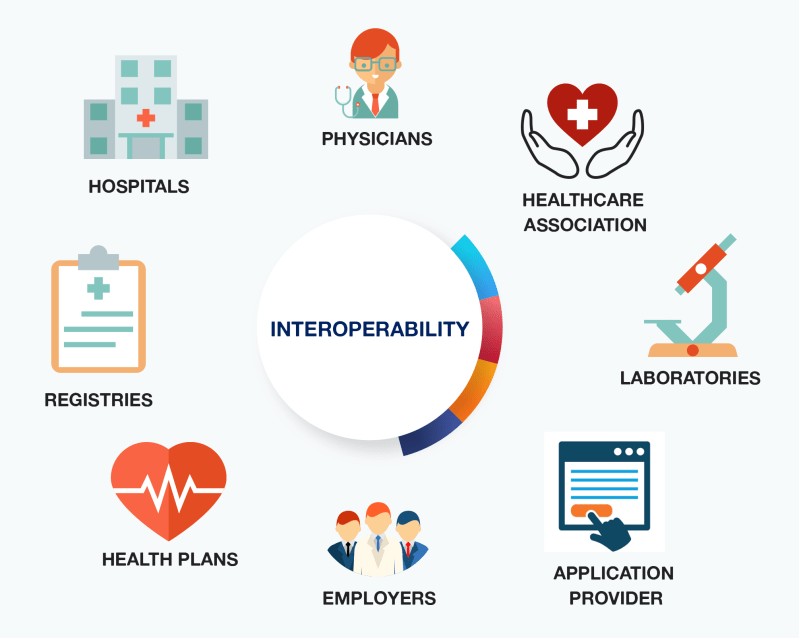
Photo By KeyReply
The Concept of Interoperability in Healthcare IT
Interoperability in healthcare refers to the ability of different information technology systems and software applications to communicate, exchange data, and use the information that has been exchanged effectively. There are several levels of interoperability:
1. Foundational interoperability allows data exchange from one information system to another without requiring the ability for the receiving system to interpret the data.
2. Structural interoperability is an intermediate step, which defines the structure or format of data exchange (syntax), ensuring that data transfers between systems can be interpreted at the data field level.
3. Semantic interoperability ensures that the transferred data is understandable and usable by the receiving system. This level of interoperability is essential for enabling access to actionable information and supporting care delivery.
The State of Healthcare IT Interoperability
Despite initiatives like the 21st Century Cures Act in the US, which mandates the free flow of health information and penalizes health IT vendors for information blocking, interoperability remains a major pain point. According to the Office of the National Coordinator for Health Information Technology (ONC), only 40% of hospitals could engage in all four domains of interoperability (send, receive, integrate, and search) in 2019. While progress has been made, significant barriers continue to impede the seamless exchange of health information.
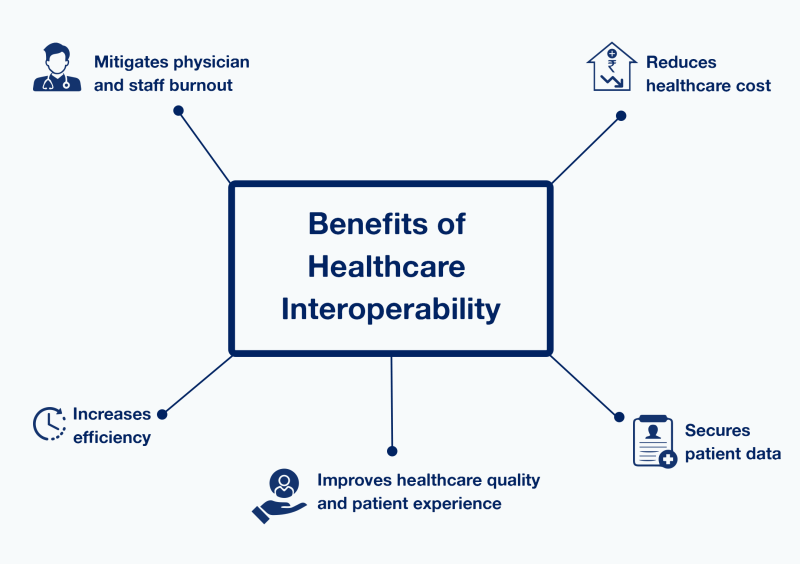
Photo By KeyReply
Key Challenges in Achieving Interoperability
1. Varied Data Standards and Formats: The lack of uniform data standards and formats is a critical barrier to interoperability. Different EHR systems often use proprietary formats, which hinders the exchange of information. For example, laboratory results or imaging reports are not always compatible across systems.
2. Information Blocking: Intentional or unintentional practices by health IT vendors and providers can prevent the sharing of health information. This may stem from a desire to protect proprietary information, a lack of understanding about data-sharing regulations, or concerns about patient privacy.
3. Complexity of Healthcare Data: Healthcare data is complex and multidimensional, including structured data such as ICD-10 codes and unstructured data such as clinician notes. Integrating these data types across diverse platforms is technically challenging.
4. Privacy and Security Concerns: Ensuring patient data privacy and security is paramount. The need to comply with regulations such as HIPAA in the US, GDPR in Europe, and other regional laws adds layers of complexity to interoperability efforts.
5. Cost and Resource Constraints: Achieving interoperability requires significant investment in terms of money and human resources. Smaller practices, in particular, may lack the necessary capital and IT expertise to upgrade their systems.
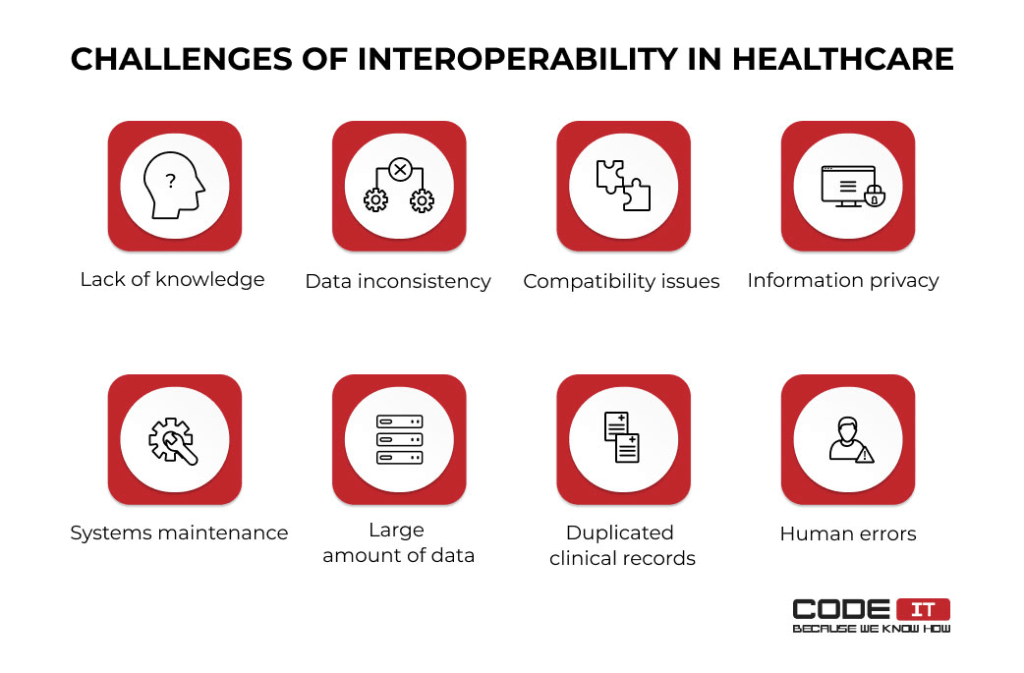
Photo By CodeIT
Implications for Operational Efficiency and Patient Care
The lack of interoperability in healthcare IT systems can lead to numerous operational inefficiencies and can negatively affect patient care in several ways:
1. Duplicate Tests and Procedures: Without access to a patient’s full medical history, healthcare providers may order redundant tests and procedures, leading to unnecessary healthcare spending and potential patient discomfort or risk. A study by the Journal of the American Medical Association (JAMA) found that the lack of interoperability leads to significant duplication of tests, costing the healthcare system billions annually.
2. Delays in Care: When healthcare providers cannot promptly access critical patient information, it can lead to delays in diagnosis and treatment. These delays can be life-threatening in emergency situations and can significantly impede the coordination of care.
3. Fragmented Patient Records: Fragmented patient records may lead to incomplete understanding of a patient’s medical history. This can result in medication errors, adverse drug interactions, and other avoidable medical errors that compromise patient safety.
4. Patient Experience: The administrative burden of coordinating records across different systems can fall on patients, especially when transferring care between providers. This can lead to frustration and decreased satisfaction with the healthcare experience.
5. Burnout Among Healthcare Providers: The additional time and effort required to navigate interoperability issues can contribute to clinician burnout. A survey by the American Medical Association (AMA) revealed that physicians who use EHRs and digital health records report high levels of burnout due to the time-consuming nature of data entry and lack of intuitive interfaces.
Photo By National Rural Health Association
Strategies for Improving Interoperability
1. Adopting Universal Data Standards: Encouraging the adoption of universal data standards, such as Fast Healthcare Interoperability Resources (FHIR), can help facilitate better data exchange. FHIR builds on previous data standards to simplify the exchange of healthcare information and supports RESTful APIs, which are widely used in other industries.
2. Supporting Open APIs: Promoting the use of open APIs allows for third-party developers to create tools that can work with various EHR systems, potentially bridging the gaps between different technologies.
3. Incentivizing Data Sharing: Government programs and payer initiatives can offer incentives for healthcare providers to share data and adopt interoperable systems. These programs can help offset the cost of transitioning to interoperable platforms.
4. Implementing Robust Data Governance: Establishing clear data governance policies can ensure that data is shared securely and in compliance with privacy laws. This includes standardizing consent processes and ensuring patients understand their rights and options regarding data sharing.
5. Investing in Training and Support: Providing adequate training and support for healthcare providers to work with interoperable systems can reduce the burden on staff and improve data quality.
Photo By CIFS Health
Interoperability in healthcare is a complex challenge with significant implications for patient care and operational efficiency. While technological and regulatory hurdles remain, concerted efforts across the industry towards adopting universal standards, incentivizing data sharing, and investing in training can pave the way for a more connected and efficient healthcare system. As we move forward, the goal of achieving true interoperability will require collaboration among healthcare providers, IT vendors, policymakers, and patients to create a healthcare ecosystem that is not only connected but also secure, user-friendly, and ultimately focused on enhancing patient outcomes.
Please leave your feedback in the comment section below.

Leave a comment